 This is the third in the four-article series on atrial fibrillation by Dr. Ahmad. The first article appeared in the June edition of Up Close, and introduced the topic of atrial fibrillation. The remaining article will address treatment options for atrial fibrillation.
This is the third in the four-article series on atrial fibrillation by Dr. Ahmad. The first article appeared in the June edition of Up Close, and introduced the topic of atrial fibrillation. The remaining article will address treatment options for atrial fibrillation.
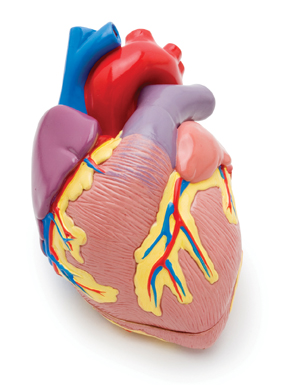
Stroke in atrial fibrillation is common, yet preventable.
Once atrial fibrillation is diagnosed and its cause is established, the next step is to assess the risk of stroke. The doctor uses several methods to evaluate the risk of stroke. However, all these methods utilize the answer to five questions and assign a score to each question.
The assessment of risk for stroke still needs sophisticated testing, but stroke in atrial fibrillation does not. The risk for stroke in atrial fibrillation is not assessed with advanced or expensive tests, but with a face-to-face interview with the doctor. Here are the five simple questions:
QUESTIONS: SCORE
1. Do you have Congestive heart failure? c 1
2. Do you have a history of Hypertension? h 1
or are you taking blood pressure medications?
3. Are you 65 years of age or older? a 1
4. Are you a diabetic? d 1
5. Do you have a previous history of stroke? s 2
Each question is assigned a score of one, except for the stroke question, bringing the total score to 6. You add up your total score. For example, a 75-year-old diabetic, with a history of previous stroke, has a CHADS SCORE 4/6. On the other hand, a 50-year-old person with heart failure and high blood pressure would have a score of only 2/6. The higher the CHADS SCORE is, the higher the risk for stroke. The annual risk for stroke with a CHADS SCORE OF 2/6 is around 4 percent a year. Compare this with the annual risk of stroke to almost 9 percent per year when the CHADS SCORE increases to 4/6. Generally, once the CHADS SCORE reaches 2 or more, blood thinners should be strongly considered.
BLOOD THINNERS ON THE MARKET
Gone are the days when Coumadin, aka Warfarin, the notorious rat poison, was the only option. There now are several drugs.
Compared to Coumadin, these new drugs are expensive, and not for people with heart valve issues or artificial valves. They have less dietary restrictions, and may not require frequent blood testing. Regardless of the blood thinner used, safety practices remain the same.
BLOOD THINNERS AND SAFETY PRACTICES
The safe use of blood thinners rests on several factors. Open communication between patient and doctor is important. Meticulous care in food intake is crucial. Increased consumption of green vegetables, including spinach and asparagus, can lower the efficacy and protective effect of the blood thinner. Similarly, some antibiotics may potentiate the effect of blood thinners, increasing the risk for bleeding.
Do not double the dose the next day because you forgot to take the blood thinner the day before. Try keeping track so you do not miss your medication. One solution is to take your medications at the same time daily. With blood thinners, precaution in the use of sharp objects or knives also goes without saying. Electric razors are generally advised.
Certain symptoms should never be ignored if blood thinners are prescribed. Always report blood in sputum, stools or urine promptly. If any part of your body, including the nose, is bleeding, or you have a sudden severe headache, don’t wait to call your doctor. Call 911.
Consider a bracelet or necklace alert, which displays that you are a blood thinner user. Lives have been saved when these have been found on patients who have been rendered unconscious by an accident, a seizure or stroke.
WE ARE NOT CREATED EQUAL
Medicine is a science, but is always practiced as an art. What is good for the goose may not be good for the gander, and vice versa. Therefore, an open conversation between you and your doctor will help weigh the pros and cons of a blood thinner. A blood thinner may be indicated in a patient with atrial fibrillation. However, a 92-year-old fragile lady, with an unsteady gait who falls easily, could experience lethal bleeding, which may outweigh benefits of the blood thinner. Such issues may require investigation. The family may visit the doctor, as well, during this decision-making process, provided the patient allows participation.
Alcohol intoxication increases the risk of falls. A blood thinner may result in serious life-threatening bleeding. Therefore, be candid with your doctor regarding your social life. Any situation increasing the risk of injury and bleeding may require discussion. Hobbies like horse riding or ATV riding also may have to be revisited, along with playing contact sports.
With a little time, effort and dedication by the patient and doctor, the risk for stroke can be minimized and controlled.
Dr. Afroze Ahmad is a multiple board certified cardiologist practicing at Las Sendas Cardiology, PC, located at 3514 N. Power Road. For information, or to make an appointment, call (480) 361-9949.

